"Everyone was nice, the tech was very nice and did part of the initial work, very gentle and thorough. Saw Dr. Voigt and he was very pleasant, finished checking things and had some good recommendations."
Sinus & Nose
Sinonasal Conditions
Office Balloon Sinus Dilation
Office Balloon Sinus Dilation now offered in Alexandria, VA
Sinusitis sufferers–find instant relief that lasts.
Office sinus dilation is a minimally invasive option that can be performed by doctors right here, in our offices. The goal of office sinus dilation is to reshape anatomy, to expand sinus pathways, and to restore drainage.
The procedure utilizes small balloons placed in key places in the nose and sinus, which are then dilated to expand the sinus pathways. It may be an effective, lasting option for some patients whose symptoms do not resolve with medication.
The benefits of office sinus dilation include:
- Delivers instant, lasting relief
- Convenient, comfortable office procedure
- Quick recovery—most patients return to normal activity in 24 hours
- May reduce healthcare costs
Discuss office sinus dilation with us today!
We are trained and experienced users of office sinus dilation technologies. Make an appointment at either of our Alexandria offices today to determine if balloon sinus dilation is right for you.
Check Patient Post Procedure Interviews
Functional Endoscopic Sinus Surgery
Sinus surgery has evolved over the last several years into a minimally invasive, outpatient procedure performed endoscopically without any external incisions. The advent of minimal to no packing in functional endoscopic sinus surgery (FESS) has led to much faster recovery times. When packing is used, gentle, dissolvable forms are available that resorb with nasal rinsing.
The technique of sinus surgery has also changed from more aggressive tissue removal, to mucosal preservation techniques that focus on finding the natural openings to the sinus cavities and widening them in a controlled manner.
Commonly used instruments include seekers and forceps, which gently find and help remove diseased tissues. Powered instrumentation called microdebriders are used cautiously to help clear nasal polyps and bony fragments that have been dissected. Image guided sinus surgery (IGSS) is a new modality that uses a CT scan or MRI to help confirm anatomic landmarks intraoperatively. IGSS can be helpful in difficult and revision sinus cases in which normal anatomic landmarks are distorted.
Potential Complications Of Endoscopic Sinus Surgery:
Minor complications
Minor complications include bleeding, pain, infection, and nasal congestion. While significant bleeding that requires a trip to the operating room for control is extremely rare, mild bleeding is a normal aspect of the post-operative course and usually resolves within 24 hours. Other minor complications are commonly and effectively treated with analgesics, antibiotics, and steroids. Scar tissue formation is a troublesome complication that can occur in the post-operative course. This can cause the newly-created sinus openings to close down and cause recurrent sinus infections. Consistent office management can help limit scar tissue formation.
Major complications
Major complications involve the brain and the eye. A cerebrospinal fluid (CSF) leak can occur when the skull base is violated They can usually be repaired endoscopically using native tissue grafts and tissue sealants. Eye complications include injury to the extraocular muscles or nasolacrimal duct and bleeding into the orbit. These rare complications may require the help of an ophthalmologist to correct.
Nasal Endoscopy
During your visit to SINOVA for a nasal or sinus issue, the practitioner may wish to perform an endoscopic examination of the nasal passageways. The nasal endoscope is a thin, rod-like camera that helps to magnify the lining of the nose. It is used to:
- Look for masses or other obstructive lesions in the portions of the passageway further back
- Perform cultures of pus/infected drainage or biopsy of lesions
- Remove crusts and debris from the sinus openings after surgery to prevent scar and infection
- Evaluate sinus anatomy after previous surgery
- Allow the patient to visualize their own nasal passageways on monitors for education purposes
After we have obtained verbal permission from you, we spray a topical anesthetic spray that will numb (Lidocaine) and decongest (Afrin) your nasal passages. Unfortunately, the spray tastes quite bitter and you may swallow some of it, thus making the throat feel numb. The good news is that it only lasts about 15 – 20 minutes. The endoscope is then passed into the nose and each passageway is carefully examined. The vast majority of patients tolerate the procedure very well. For more information on nasal endoscopy, refer to:
American Rhinologic Society Patient Care
Nasal Polyps
Nasal polyps are benign lesions that occur within the lining of the nasal and sinus cavities. They are the end result of inflammatory processes that present as translucent grape-like structures.
Symptoms include nasal congestion, difficulty or inability to smell, and occasionally, bleeding. Nasal polyps can block the natural openings of the sinuses and cause sinusitis.
We do not completely understand how and why nasal polyps form. Multiple theories exist, including allergy and blood vessel permeability, but studies have not shown a single one to be definitive. Nasal polyps are associated with a number of conditions such as asthma, cystic fibrosis, and allergic fungal sinusitis.
Treatment of nasal polyps involves both medical and surgical therapy. Saline irrigations, nasal steroids, oral steroids, antibiotics, topical steroid irrigations, mucolytics, and leukotriene modifiers are some of the medications used to manage nasal polyps. Functional endoscopic sinus surgery is the mainstay of surgical management.
Septal and Turbinate Procedures
The nasal septum is the partition that divides one side of the nose from the other. It is rarely perfectly straight–it is slightly crooked in over 80% of people. When the septum is so crooked or deviated that it blocks the nasal passage, then a surgical operation called a septoplasty may restore clear breathing. Please check out the link below for more information.
American Rhinologic Society Patient Care
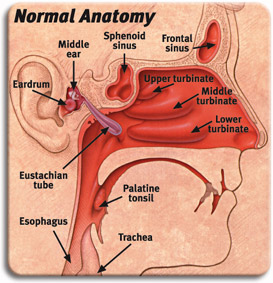
Sinus Anatomy
The main structures of the nasal passages are the sinuses, the septum, and the turbinates.
The sinuses are hollow, air-filled cavities that are located within the bones that comprise the skull. There are four paired structures consisting of:
- Maxillary sinuses – located behind the cheek
- Ethmoid sinuses – small honeycomb-shaped cells located between the eyes
- Frontal sinuses – located behind the forehead
- Sphenoid sinuses – located behind the nasal passageway near the brain.
It is unclear as to the definitive function of the sinuses but they may play a role in voice resonance, humification of inspired air, and as a shock absorber for the head. All of the sinuses have openings that communicate with the nasal passageways. The sinuses have a mucosal lining that produces mucus and contains cilia, which are tiny, microscopic hair-like structures that play an important role in clearing the mucus. Cilia beat in conjunction to sweep the mucus, which traps bacteria and allergens, into the nasal passageways and into the throat. Studies have shown that cilia function best in a warm, moist environment.
The turbinates are tubular structures that are bony outgrowths covered with a thick mucosal lining. This lining contains a rich blood supply, which allows the turbinates to perform the important function of warmth and humification of inspired air as it proceeds into the lungs. A secondary function is to trap bacteria and allergens as they initially enter the body. This exposure to allergens can often cause swelling of the turbinates (turbinate hypertrophy), which is a frequent cause of nasal congestion.
The nasal septum is the wall that separates the right and left nasal passageways. The septum is comprised of mostly cartilage in the front of the nose, and bone in the back. It is lined by a mucosal lining on both sides, which contains its blood supply. Septal deviation is a common finding in which a part of the septum bends toward either the left or right. At times, the deviation can cause nasal obstruction, headaches, and even sinusitis by blocking the openings.
Sinusitis
Sinusitis is defined as inflammation of the sinuses caused by a number of etiologies including bacteria, viruses, fungi, pollutants, nasal polyps, anatomic abnormalities, and allergies among other agents.
The above agents cause swelling of the sinonasal lining. The sinuses produce roughly 1 liter of mucus daily that is cleared by the cilia. When the lining is swollen, the cilia do not function properly and the mucus becomes stagnant. This eventually leads to blockage of the openings of the sinuses and a vicious cycle begins leading to bacterial colonization of the mucus and thus, sinusitis.
Symptoms of sinusitis can be divided into major and minor symptoms. The diagnosis of sinusitis requires at least 2 major or 1 major and 2 minor symptoms.
Major Symptoms
- Nasal drainage
- Post nasal drainage
- Facial pain and/or pressure
- Nasal obstruction and/or congestion
- Decreased ability to smell
- Headache
Minor Symptoms
- Fever
- Cough
- Fatigue
- Upper teeth pain
- Ear pressure and/or fullness
- Headache
Sinusitis can be classified into 4 categories:
- Acute: Symptoms that last up to 4 weeks with complete resolution
- Subacute: Symptoms that last between 4 and 12 weeks with complete resolution
- Recurrent Acute: 4 or more episodes per year with resolution of symptoms between episodes
- Chronic: Symptoms occurring for 12 or more weeks
Nose
Nosebleeds
Anterior nosebleeds are common in dry climates or during the winter months when dry, heated indoor air dehydrates the nasal membranes. Dryness may result in crusting, cracking, and bleeding. This can be prevented by placing a light coating of petroleum jelly or an antibiotic ointment on the end of a fingertip and then rub it inside the nose, especially on the middle portion of the nose (the septum).
How To Stop An Anterior Nosebleed?
- Stay calm, or help a young child stay calm. A person who is agitated may bleed more profusely than someone who’s been reassured and supported.
- Keep head higher than the level of the heart. Sit up.
- Lean slightly forward so the blood won’t drain in the back of the throat.
- Using the thumb and index finger, pinch all the soft parts of the nose or place a cotton ball soaked with Afrin, Neo-Synephrine, or Dura-Vent spray into the nostril and apply pressure. The area where pressure should be applied is located between the end of the nose and the hard, bony ridge that forms the bridge of the nose. Do not pack the inside of the nose with gauze or cotton.
- Apply ice—crushed in a plastic bag or washcloth—to nose and cheeks.
- Hold the position for five minutes. If it’s still bleeding, hold it again for an additional 10 minutes.
What Are The Causes Of Recurring Nosebleeds?
- Allergies, infections, or dryness that cause itching and lead to picking of the nose.
- Vigorous nose blowing that ruptures superficial blood vessels.
- Clotting disorders that run in families or are due to medications.
- Drugs (such as anticoagulants or anti-inflammatories).
- Fractures of the nose or the base of the skull. Head injuries that cause nosebleeds should be regarded seriously.
- Hereditary hemorrhagic telangiectasia, a disorder involving a blood vessel growth similar to a birthmark in the back of the nose.
- Tumors, both malignant and nonmalignant, have to be considered, particularly in the older patient or in smokers.
Tips To Prevent A Nosebleed:
- Keep the lining of the nose moist by gently applying a light coating of petroleum jelly or an antibiotic ointment with a cotton swab three times daily, including at bedtime. Commonly used products include Bacitracin, A and D Ointment, Eucerin, Polysporin, and Vaseline.
- Keep children’s fingernails short to discourage nose picking.
- Counteract the effects of dry air by using a humidifier.
- Use a saline nasal spray to moisten dry nasal membranes.
- Quit smoking. Smoking dries out the nose and irritates it.
Tips To Prevent Rebleeding After Initial Bleeding Has Stopped:
- Do not pick or blow nose.
- Do not strain or bend down to lift anything heavy.
- Keep head higher than the heart.
If Rebleeding Occurs:
- Attempt to clear nose of all blood clots.
- Spray nose four times in the bleeding nostril(s) with a decongestant spray such as Afrin or Neo-Synephrine.
- Repeat the steps to stop an anterior nosebleed.
Call a doctor if bleeding persists after 30 minutes or if nosebleed occurs after an injury to the head.
Mouth
Smell & Taste
Four basic taste sensations give “flavor” to life:
- Sweet
- Sour
- Bitter
- Salty
Certain combinations of these tastes – along with texture, temperature, odor, and the sensations from the common chemical sense – produce a flavor. It is flavor that lets us know whether we are eating peanuts or caviar.
Many flavors are recognized mainly through the sense of smell. If you hold your nose while eating chocolate, for example, you will have trouble identifying the chocolate flavor – even though you can distinguish the food’s sweetness or bitterness. This is because the familiar flavor of chocolate is sensed largely by odor. So is the well-known flavor of coffee. This is why a person who wishes to fully savor a delicious flavor (e.g., an expert chef testing his own creation) will exhale through his nose after each swallow.
Taste and smell cells are the only cells in the nervous system that are replaced when they become old or damaged. scientists are examining this phenomenon while studying ways to replace other damaged nerve cells.
Are Smell And Taste Disorders Serious?
Smell and taste problems can have a big impact on our lives. Because these senses contribute substantially to our enjoyment of life, our desire to eat, and be social, smell and taste disorders can be serious. When they are impaired, life loses some zest; we eat poorly, socialize less, and as a result, feel worse. Many older people experience this problem.
Smell and taste also warn us about dangers, such as fire, poisonous fumes, and spoiled food. Certain jobs require these senses to be accurate – chefs and firemen rely on taste and smell. One study estimates that more than 200,000 people visit a doctor with smell and taste disorders every year, but many more cases go unreported.
Loss of the sense of small may be a sign of sinus disease, growths in the nasal passages, or, in rare circumstances, brain tumors.
What Can I Do To Help Myself?
If you experience a smell or taste problem, try to identify and record the circumstances surrounding it. When did you first become aware of it? Did you have a “cold” or “flu” then? A head injury? Were you exposed to air pollutants, pollens, danders, or dust to which you might be allergic? Is this a recurring problem? Does it come in any special season, like hay fever time?
Bring all information with you when you visit a physician who deals with diseases of the nose and throat. Also be prepared to tell him about your general health and any medications you are taking. Proper diagnosis by a trained professional can provide reassurance that your illness is not imaginary. You may even be surprised by the results. For example, what you may think is a taste problem could actually be a smell problem, because much of what you think you taste you really smell.
Diagnosis may also lead to treatment of an underlying cause for the disturbance. Many types of smell and taste disorders are reversible, but if yours is not, it is important to remember that you are not alone: thousands of other patients have faced the same situation.
Can Smell And Taste Disorders Be Treated?
Sometimes a certain medication is the cause of a smell or taste disorder, and improvement occurs when that medicine is stopped or changed.
Although certain medications can cause chemosensory problems, others – particularly anti-allergy drugs – seem to improve the senses of taste and smell.
Some patients – notably those with serious respiratory infections or seasonal allergies – regain their sense of smell or taste simply by waiting for their illness to run its course. In many cases, nasal obstructions such as polyps can be removed to restore airflow to the receptor area and can correct the loss of smell and taste. Occasionally, chemosenses return to normal just as spontaneously as they disappeared.
How Do Smell And Taste Work?
Smell and taste belong to our chemical sensing system (chemosensation). The complicated processes of smelling and tasting begin when molecules released by the substances around us stimulate special nerve cells in the nose, mouth, or throat. These cells transmit messages to the brain, where specific smells or tastes are identified.
Olfactory (smell nerve)
Cells are stimulated by the odors around us – the fragrance from a rose, the smell of bread baking. These nerve cells are found in a tiny patch of tissue high up in the nose, and they connect directly to the brain.
Gustatory (taste nerve)
Cells react to food or drink mixed with saliva and are clustered in the taste buds of the mouth and throat. Many of the small bumps that can be seen on the tongue contain taste buds. These surface cells send taste information to nearby nerve fibers, which send messages to the brain.
The common chemical sense
Another chemosensory mechanism, contributes to our senses of smell and taste. In this system, thousands of free nerve endings – especially on the moist surface of the eyes, nose, mouth, and throat – identify sensations like the sting of ammonia, the coolness of menthol and the “heat” of chili peppers.
What Causes Smell And Taste Disorders?
Scientists have found that the sense of smell is most accurate between the ages of 30 and 60. It begins to decline after age 60, and a large proportion of elderly persons lose their smelling ability. Women of all ages are generally more accurate than men in identifying odors.
Some people are born with a poor sense of smell or taste. Upper respiratory infections are blamed for some losses, and injury to the head can also cause smell or taste problems.
Loss of smell and taste may result from polyps in the nasal or sinus cavities, hormonal disturbances, or dental problems. They can also be caused by prolonged exposure to certain chemicals such as insecticides and by some medicines.
Tobacco smoking is the most concentrated form of pollution that most people will ever be exposed to. It impairs the ability to identify odors and diminishes the sense of taste. Quitting smoking improves the smell function.
Radiation therapy patients with cancers of the head and neck later complain of lost smell and taste. These senses can also be lost in the course of some diseases of the nervous system.
Patients who have lost their larynx or “voice box” commonly complain of poor ability to smell and taste. Laryngectomy patients can use a special “bypass” tube to breathe through the nose again. The enhanced air flow through the nose helps smell and taste sensation to be re-established.
How Are Smell And Taste Disorders Diagnosed?
The extent of loss of smell or taste can be tested using the lowest concentration of a chemical that a person can detect and recognize. A patient may also be asked to compare the smells or tastes of different chemicals, the intensities of smells or taste of different chemicals, or how the intensities of smells or tastes grow when a chemical’s concentration is increased.
Smell
Scientists have developed an easily administered “scratch and sniff” test to evaluate the sense of smell.
Taste
In taste testing, the patient reacts to different chemical concentrations: this may involve a simple “sip, spit, and rinse” test, or chemicals may be applied directly to specific areas of the tongue.
Allergy
Allergy – Introduction
An allergy is a genetic condition causing the body to respond to harmless substances in the environment as though they were dangerous invaders. This response produces symptoms that may be mild to life-threatening in susceptible people. It occurs after a person with allergic tendencies is repeatedly exposed to the substance in his/her environment or his/her diet.
When the allergic person comes into contact with the offending substance, the body’s immune system rushes to the rescue and begins to produce antibodies to fight off the invader. These antibodies alter the way in which the body reacts, and may produce allergic symptoms.
Below is a list of common allergic symptoms based on each specific body part:
- Nose: runny nose, congestion, post nasal drip, thick mucus, pain, sneezing
- Eyes: watery eyes, itchy eyes, redness, blurred vision
- Throat: sore throat, scratchy throat, lump in throat
- Skin: rash, itching
- Lungs: wheezing, shortness of breath, exercise intolerance
Stomach/GI: diarrhea, pain
Frequently Asked Questions
Is There A Name For These Offending Substances?
They are called allergens.
What Kinds of Things Are Allergens?
Anything to which a person becomes allergic is an allergen. Certain substances, because of their physical and chemical structure are more likely to become allergens than others. Prime examples are ragweed and other pollens, and penicillin. Others are dust, mold spores, animal dander, feathers, cereal grains, some air-borne chemical pollutants, drugs and insect venoms.
What Are The Most Common Allergic Symptoms?
The most common allergic symptoms are hay fever, asthma and eczema.
What Is Hay Fever?
“Hay fever” was named because of nasal symptoms developing during hay season, but most nasal allergies are called “hay fever”. In “hay fever”, the lining of the nose becomes irritated, causing the sufferer to sneeze and the nose to become stuffed-up or to run. Eyes may itch or turn watery. Sometimes the ears feel blocked up. “Hay fever” occurs most frequently during the spring, summer or fall when trees, grasses and weeds produce pollen. One of the principal offenders is the ragweed plant which produces pollen from late summer until frost.
What Is Asthma?
Asthma is a condition which affects breathing and the lungs. The patient wheezes, coughs, and is short of breath.
What Is Eczema?
Eczema is an inflammation of the skin. It can take the form of red patches, crusts and scales. The affected area generally itches. The condition generally occurs from eating certain foods.
Do All Allergic Responses Fall Into One Of These Categories?
No. In addition to hay fever, asthma and eczema, there can be a wide range of allergic reactions suffered in all parts of the body. For example, headaches, hives, diarrhea and stomach distress can be the result of allergy.
Is An Allergy Really A Serious Illness?
An allergic reaction can be slight and annoying or very serious. The inflamed lining of the nose of someone who suffers from hay fever can become infected, making the symptoms worse. Most dangerous of all is a sudden, heavy dose of an allergen, especially one like a bee sting or drug injection. This can trigger a generalized allergic reaction bringing on collapse or even death.
Are Allergies Inherited?
While specific allergies themselves are not inherited, the tendency towards allergies is. The more allergic one’s family is, the more likely one is to develop allergies. Though the trend to develop allergies may not appear in all members of a family or even in every generation of a family, the tendency is still there.
Are Allergies Common?
It is estimated that at least 20% of the population is likely to develop some kind of allergy.
At What Age Is A Person Most Likely To Develop An Allergy?
It is most common for allergies to begin in childhood, but it is quite possible for allergic symptoms to make their first appearance at any age. You’re never too old to develop an allergy.
Can An Allergy Be Outgrown?
It is common for people to change the way their other allergic symptoms affect them, especially in childhood. For example, a baby may develop colic or eczema or have recurrent ear infections, but as it grows older, it may develop other allergic symptoms such as hay fever, ear fluid or asthma. Adults may have many varied symptoms such as chronic post nasal drainage, rashes, and stomach and intestinal problems. Older patients still have a tendency to have allergic symptoms, although they may become less noticeable with maturity.
What Causes A Person To Develop An Allergy?
There is no standard way for an allergy to begin, and the onset may be sudden or gradual. For a person to become allergic to a substance, he/she must be exposed to it more than once, and generally that exposure is quite frequent. Often, symptoms develop after an unusual stress to the immune system, such as following a severe viral infection.
If I Have An Allergy, Should I Be Treated By An Allergist?
Because allergies can produce such a wide range of symptoms, there are a number of doctors, both specialists and general practitioners, in addition to allergists, who may be qualified to treat the allergic patient. For example, a skin allergy can be effectively treated by a dermatologist (a doctor who specializes in treating skin diseases) and an infantile cow’s milk allergy may be treated by the child’s own pediatrician. An internist who is concerned with lung disease may also be involved with allergies that affect the lungs. An allergist may be any physician trained in the diagnosis and treatment of allergies. There are general allergists who treat allergies throughout the body and specialty allergists such as otolaryngologists (ear, nose and throat specialists), who specialize in a specific part of the body.
Should An Otolaryngologist Treat My Allergies?
An otolaryngologist is a doctor specializing in the treatment of ear, nose and throat diseases. Half of the problems he/she encounters are probably due, either directly or indirectly, to allergy. Chronic nasal congestion and post nasal drip, seasonal or constant, is often allergic and may be complicated by chronic sinus and middle ear disease. Hearing loss, dizziness, headaches, weeping ear canals, and chronic sore throats may be due to allergy. The otolaryngologist who does his/her own allergy treatment is able to follow the patient’s progress with specialized examinations and nose and throat medical and surgical treatment, such as polyp removal, placement of middle ear ventilating tubes, straightening of the nasal septum, and treatment of sinus infections. An otolaryngologist not providing allergy care may refer you to a colleague for such care.
What Is The First Treatment For Allergies?
First of all, a careful history of the allergic person is taken. The most basic treatment, once an allergen has been identified, is to eliminate it. This may mean giving away a pet, avoiding certain jewelry and cosmetics, deleting certain foods from the diet, and alerting physicians about drug allergies.
What If The Allergen Can’t Be Eliminated?
In the case of an allergen in the environment, such as dust, pollen, and mold, a thorough house cleaning, along with other careful preventive measures, will cut down on the exposure. However, if the allergen is seasonal pollen, moving may not be the solution since there might be tree or weed pollens in the new location which could bring about the development of another, equally distressful allergic reaction. Nasal rinses can be very helpful in limiting the allergy symptoms by cleansing the nasal passageways of the allergens.
Then Are Drugs The Answer?
Drug treatment has long been a cornerstone of allergy treatment. Antihistamines and/or decongestants (for the nose) and bronchodilators (for asthma) counteract the symptoms caused by the main chemical released by the body’s immune system in an allergy attack. There are other drugs, both pills and nasal sprays, which can prevent the release of these inflammatory chemicals or suppress the immune reactions themselves.
What About Cortisone?
Steroids of the cortisone family can suppress allergic reactions, but often there is the risk that the patient may develop significant side effects. Newer steroid nose sprays will often relieve allergies and not cause the side effects.
What About Allergy Shots?
Injections (immunotherapy) have been a satisfactory treatment for many inhaled allergens (that is, pollens, dust, molds and animal dander) and for bee stings. Before immunotherapy is begun, allergy tests are done in order to determine the offending allergens.
What Do The Allergy Shots Involve?
The patient is given small doses of his allergens by injection on a regular basis, usually weekly.
Is There A Standard Dosage For Everyone?
No. The appropriate allergens and their doses must be determined individually for each patient. Skin testing (placing a minute amount of the allergen under the skin) and the RAST (blood test for specific allergies) are both widely used for this purpose. Both detect the substances to which a person is allergic, as well as the degree of sensitivity, which helps determine the initial treatment dose.
How Long Will I Have To Take Shots?
The injections can bring significant relief within a few months. They are usually continued for 2 to 3 years. In some cases, unfortunately, it may be necessary to continue the treatment indefinitely.
How Successful Is This Treatment?
Over 80% of the patients who receive regular shots experience significant improvement or complete relief of their symptoms.
Allergy – In Vitro Testing
The term “In Vitro” refers to test procedures performed “outside the body,” as in a laboratory, as opposed to “In Vivo” procedures performed in or on the body directly, as when allergy skin tests are performed. The allergic reaction is complex. It parallels the way the body defends itself against viruses and other dangerous “foreign” invaders. Just as an antibody recognizes a virus and attaches itself to it so it may be eliminated, a substance in human blood called immunoglobulin E (IgE) also recognizes and attaches itself to allergens – the substances such as dust and pollens, which cause inhalant allergies. (Inhalants are substances which you take into your body by breathing. These include dust, pollens, molds, animal dander and tiny microscopic organisms called mites.)
Just as there are specific antibodies produced for each specific virus, specific IgE is produced for each allergen. That is, there is one type of IgE specifically for ragweed pollen, another for rye grass pollen, etc. If you have enough of a specific form of IgE in your body to cause a reaction when you breathe in one of these substances, you have an allergy.
During the first stage of allergic reaction, IgE attaches to a special cell in the tissue called the mast cell. This combination forms an allergy “bomb” that is triggered only if it contacts the IgE specific allergen. When this “bomb” explodes, it releases many chemicals, including histamine, which causes the watery eyes, runny nose, congested nose, itchy throat, and the other typical symptoms of inhalant allergies. The more the specific IgE you have, the more allergic to the allergen you are, and the stronger your body’s reaction is when you breathe it.
The key to finding out what inhalants you are allergic to is to discover what specific types of IgE are present in your blood, and how much of each type is present. That sounds simple, except that we are dealing with microscopic particles which cannot be seen by the eye or identified even with the most powerful microscopes. We have to locate and measure them by very sensitive chemical tests. And that is where these In Vitro tests come in.
In Vitro tests sound very complicated, but actually they are mechanically fairly simple. Here’s how they work:
As was mentioned, every allergic patient makes specific IgE to each allergen that they are allergic to. So if a drop of their blood serum or plasma (the liquid part of the blood that has been separated from the heavy blood cells) is combined with a drop of allergen, and specific IgE antibodies in the serum will attach to the allergen. In the In Vitro tests, the allergen to be tested is bound to plastic or paper, to which the serum is added.
The IgE is measured by adding a weak radioactive marker in the test tube (the Radio-allergo-sorbent test or RAST) or a chemical marker that will produce a color change (the enzyme linked immuno sorbent assay or ELISA test). These markers themselves may then be measured.
Using a tiny amount of blood serum, this test can be repeated to measure numerous allergens. This test is only recommended for inhalant allergens, as other problem substances such as foods do not usually involve IgE, and have to be tested in other ways. However, there may be some special circumstances for which your doctor orders these tests for food allergens as well.
Although the results of In Vitro tests are not available immediately, as are skin tests, they offer the convenience of requiring only one sample of blood to obtain the results for several different allergens. This is especially advantageous for children, as their discomfort is minimized.
RAST tests are very precise. As they indicate how allergic you are to each substance, they help guide your doctor to select a safe initial injection dose. If you are highly allergic to an allergen, your starting doses will be weaker than for those allergens to which you are less sensitive. This allows your treatment vials to be “tailor made” only for you. Older methods of testing could not measure the degree of sensitivity to each allergen before treatment is started. Because of this, it would often require more injections and a longer period of time to reach a therapeutic dose than with In Vitro testing. In Vitro testing can also be as cost effective as the older methods of skin testing.
In Vitro testing is extremely simple for the patient. After a thorough physical examination, your doctor will ask you to fill out a “patient history” form concerning the type and timing of your symptoms, to determine the most likely allergens you may be sensitive to, so these may be tested. Your home and work environment (pets, trees, plants, etc.) may provide important clues as to which allergens should be tested. It is unnecessary to test for allergens to which you are not frequently exposed.
Next, a sample of blood will be drawn from your arm. The blood sample is sent to a trained laboratory technician for testing. The laboratory sends your doctor a report indicating what allergens you are sensitive to, and how allergic you are to them. After explaining the results to you, your doctor will recommend a program to deal with your allergies. This may include changing your environment (such as eliminating offending substances around your home), medications, or taking allergy injections. With proper management, most symptoms of allergies can be very well controlled.